Dear Providers and Staff,
Not surprising, we are now clearly on the upswing of another COVID surge.
Communal Eating
Your safety is our top priority. Recently, we’ve had several COVID exposures among vaccinated individuals during conferences which could have been avoided if they were simply sitting six feet apart while eating. Per Dr. Henrich, not only should we not share meals, but we should not sit together while eating (i.e. avoid communal eating). Although we are still allowing in-person gatherings, video meetings are preferred. Also, we strongly encourage you to wear your mask even if you are vaccinated. We want to maintain our educational activities and open dining, but to do that, we must do it safely.
On a similar note, I’m highly impressed by the great work-ethic here, but when sick, please stay home and get tested for COVID. The health and wellbeing or your coworkers depend on it. Directions for testing are provided at the bottom of this message.
Inpatient Care at University Hospital
Once again, our Medicine services and ICU beds are filling with COVID patients. I ask other services to help unload the Medicine services by keeping patients on their own service with Medical Consultation.
As the surge progresses, we will do our best to maintain elective in-patient procedural cases, but that also means we need to avoid canceling cases or postponing cases from the weekend to the work week. We also need to use all the OR times (such as Friday afternoons).
Thank you
Thank you to the Department PM&R for once again vacating your space at Reeves in order to accommodate sick COVID patients. That comes at no small cost to your mission and training program. As noted, our Emergency Medicine, Hospitalist, as well as Critical Care providers are once again mobilizing for the surge as well. The number of sacrificial actions taken during this pandemic continue to impress me, and they are so numerous it’s easy to overlook them. Please remember to thank them all (and others) for their intrepid contributions. In the meantime, the best thing we can do for them is to help get the public fully vaccinated as well as prevent those infected with COVID from becoming severely ill! That leads to my next two topics…
Vaccine Hesitancy Best Practice Advisory (BPA)
Starting next week for all UTHP clinics, BPAs will alert MAs during patient clinic visits for those who do not have their COVID vaccination series documented in Epic. The MA can satisfy the BPA by either documenting prior vaccination or indicating the patient agrees to the vaccine (staff are not ordering the vaccine at this point). If the MA cannot satisfy the BPA, then another BPA will alert the provider upon opening the chart, giving the provider the opportunity to discuss this with the patient. Good data shows provider endorsement enhances vaccination acceptance. Informational posters are being distributed to all clinics and can be accessed here and here.
Monoclonal Antibody Infusions
The goal of Monoclonal Antibody treatment is to help reduce the likelihood that a high-risk COVID patient will progress to severe disease/hospitalization. The referral form and information about monoclonal antibody infusions can be found on https://strac.org/ric. The guidelines are fairly liberal for which patients are considered high enough risk to merit referral: obesity, age >65, diabetes, chronic kidney disease, cardiovascular disease, immunosuppressive conditions or treatments, and even being a high-risk ethnicity (latino or black) can be qualifying conditions. The patient must have a documented positive COVID test, must be less than 10 days since symptom onset (and the earlier, the better), and must have an oxygen saturation >93% on room air (ie, they must not ALREADY HAVE severe disease). Currently, the infusions are being administered via a mobile unit, at the patient's homes.
The referral form is easy to complete, and should be emailed to infusionreferral@bcfs.net (note: on the form itself, it says to email to "refer@strac.org," but this is no longer functional - the website has been updated with the correct email address, but the form itself has not been).
I encourage our ambulatory providers who are seeing this patient population (newly-diagnosed, early in the disease course, still not requiring oxygen, high-risk conditions) to refer them for this treatment. It could help them as well as reduce strain on our ED and inpatient services.
COVID-19 Booster Shots
This is a hotly debated item. However, at this time it is not recommended by the CDC, FDA, or WHO. Stay tuned. Once it is approved, it will be a big deal, and we will let you know.
COVID Surge
As noted in the figure below, the inpatient COVID census has more than doubled over the past few weeks.
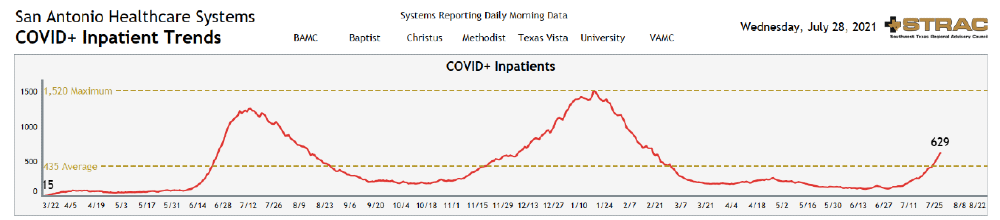
Predictive models estimate the COVID census will likely double again over the next month and then start to drop off.
We do not anticipate the inpatient non-COVID census will decrease, so we are bracing for some very high volumes at University Hospital, including the Emergency Center.
Plans are being put in place to mitigate these higher volumes.
- If you need to send a patient to UH Emergency Center, please always use the UH One Call Center number: 210-743-3100. You will be promptly connected with an EM Attending who will help facilitate the care of your patient.
- UH has currently converted or added over 20 inpatient medicine beds.
- UH/UT are working to implement a Hospital at Home (H@H) Program. There is a strong body of literature to support H@H, so I suspect this may become an enduring effect after the pandemic, similar to Telehealth and mRNA vaccines. Yet in the meantime and even after H@H is implemented, early discharges is still a top priority.
Additionally:
- If you are not yet vaccinated, we strongly encourage you to do so.
- Whether vaccinated or not, please continue to wear your mask in all clinical locations, and we strongly encourage you to wear them on campus as well.
- We are actively reviewing/updating all UTHP COVID mitigation protocols.
- If you need a COVID test:
- Employees and students: Please contact Wellness 360 at COVID-19@uthscsa.edu or visit the COVID-19 Testing website for more information.
- Residents: Please contact UH Employee Health at 210-358-9999 or at employee.health@uhs-sa.com for instructions.
As always, with deepest gratitude, thank you for all you are doing,
Bob Leverence, MD, FACP
Chief Medical Officer
UT Health Physicians